Stroke Protocol – DW/Flair Perfusion
Up to 25% of stroke patients wake up with a neurological deficit, so called wake-up stroke (WUS). Different imaging approaches that may aid in the selection of patients likely to benefit from reperfusion therapy are currently under investigation. The magnetic resonance imaging (MRI) diffusion weighted imaging – fluid attenuated inversion recovery (DWI-FLAIR) mismatch concept is one proposed method for identifying patients presenting within 4.5 hours of the ischemic event.
Multimodal MRI can delineate the presence, size, location, extent and effects of acute brain ischemia, identify the hypoperfused tissue that is at risk of infarction, and show additional features of the cerebrovascular pathology
A typical acute stroke MRI protocol includes the following sequences : diffusion-weighted imaging (DWI), gradient-recalled echo (GRE), T2-weighted fluid-attenuated inversion recovery (FLAIR), magnetic resonance angiography (MRA), and perfusion-weighted DWI has transformed the diagnosis of ischemic stroke imaging (PWI).
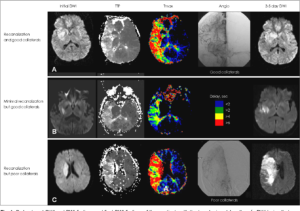
The patient arrived at the emergency room 45 min after symptom onset. MRI was started 20 min later, and the patient was treated with intravenous tissue plasminogen activator 55 min after arrival. DWI sequence showed an area of hyperintensity in the right temporal, insular and frontal lobes.
Apparent diffusion coefficient map showed a matching area of hypointensity, confirming that the DWI lesion was due to acute ischemia.
Fluid-attenuated inversion recovery showed no matching hyperintensity, indicating that the DWI lesion was
Contrast-enhanced MRA of the neck and brain revealed a chronic asymptomatic right carotid occlusion, although the patient had good collateral flow through the anterior communicating artery, and his right carotid artery was normal.
Diffusion-weighted Imaging
DWI has transformed the diagnosis of ischemic strokein its earliest stages, from reliance on a mostly clinical inference about the presence, localization and size of an ischemic lesion to imaging confirmation of the infarct.
This technique is the only brain imaging method to reliably demonstrate ischemic parenchymal injury within the first minutes to hours after onset.
Ischemia-induced membrane dysfunction and cytotoxic edema restrict the diffusion of water and lead to a decrease in the apparent diffusion coefficient (ADC), a physiological measure of the rate of water movement through brain parenchyma. DWI is an ideal sequence for imaging patients with acute stroke. In a prospective, blinded comparison of non-contrast CT and MRI in a consecutive series of patients referred for emergency assessment of suspected acute stroke, the sensitivity of DWI for ischemic acute stroke ranged from 73% (3 h after the event) to 92% (>12 h after the event). By contrast, the sensitivity of CT at these times was 12% and 16%, respectively. The specificity of MRI for stroke detection was 92% (at 3 h) and 97% (>12 h).
Perfusion-weighted Imaging
PWI visualizes capillary blood flow and, thus, can demonstrate the presence of cerebral ischemia. The most commonly used MRI method to study cerebral perfusion in clinical practice and research is dynamic susceptibility contrast-enhanced imaging. In this technique, a gadolinium-based contrast agent is injected as an intravenous bolus. Gadolinium is paramagnetic and, therefore, has a local susceptibility effect that can be detected with T2-weighted or T2*-weighted imaging as a drop in signal intensity. Repeated series of susceptibility-weighted, T2*-weighted images are acquired for several seconds before and after the injection of the gadolinium bolus to track the signal change.
Interpretation of the source PWI images is an alternative option when hemodynamic maps are not available or are affected by patient motion. PWI source images are T2* weighted and can, therefore, be used to confirm (or identify, if a GRE sequence is not available) the presence of ICH or an intravascular thrombus.

